Why do I have risk of stroke?
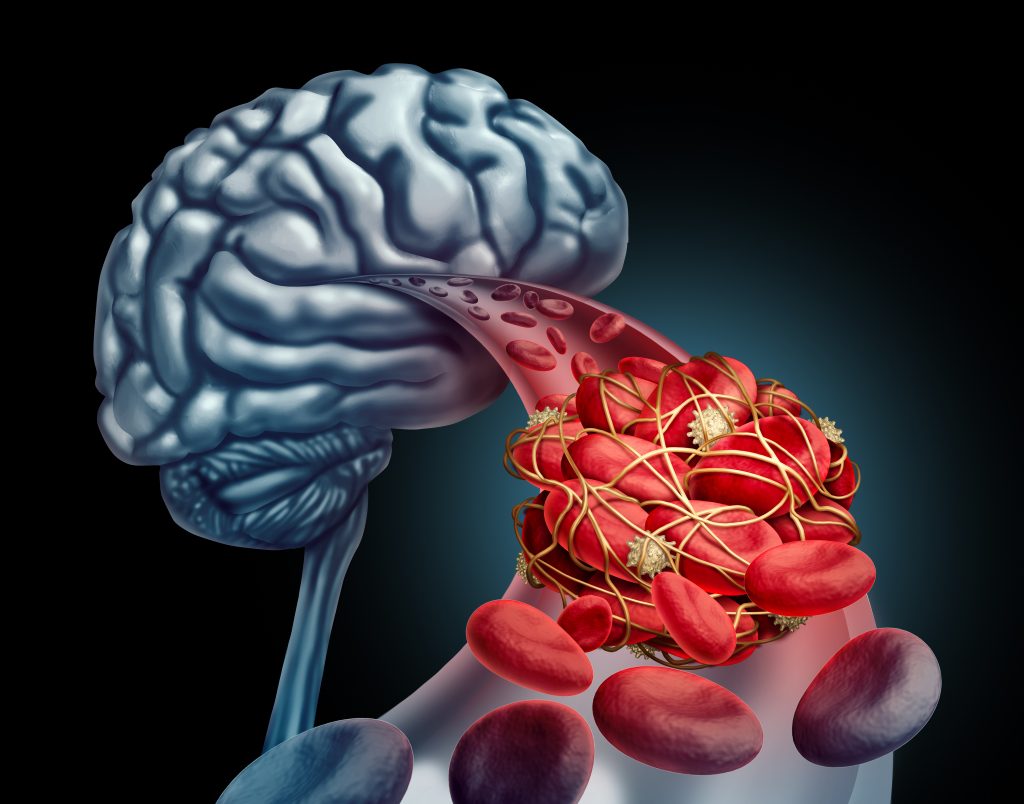
In atrial fibrillation the atrial contraction is diminished, causing slowing or even stagnation of blood flow, which can lead to clot formation. This clot can then be released into the circulatory system leading to stroke or systemic embolism. The risk of clot formation is higher if certain comorbidities as for example high blood pressure or higher age are present. To prevent stroke in patients with a higher risk, medications colloquially called “blood thinners” (anticoagulants) are usually recommended. Your physician will calculate your risk and discuss with you the advantages and possible risks of taking a blood thinning medication. You should decide together (“shared decision-making”) whether you start such a medication, or not.
To learn more about shared decision-making for anticoagulation and why is it important for you to take an active part in the decision, please read the following article specifically written for patients:
Patients, family members, and health professionals making decisions together about starting blood thinning treatment to prevent stroke in patients with an irregular heart rhythm” (European Journal of Cardiovascular Nursing, Science for Patients).
What is my risk of stroke?
Your doctor has probably discussed the risk of having stroke associated with atrial fibrillation. This is calculated using a score named CHA2DS2- VASc – score. The following conditions increase your risk; congestive heart failure – 1 point, high blood pressure – 1 point, age ≥ 65 – 1 point, ≥ 75 – 2 points, diabetes – 1 point, previous stroke or transitory ischemic attack – 2 points, vascular disease (peripheral arterial disease, previous myocardial infarction, aortic atheroma) – 1 point and female gender also counts for 1 point.
According to the number of points and therefore CHA2DS2- VASc – score, the risk of stroke rises from 1.3% yearly (if CHA2DS2- VASc – score =1), to 15.2% yearly (if CHA2DS2- VASc – score = 9).
Assessing your risk of stroke, if you have atrial fibrillation – online calculator
Some people have attacks of atrial fibrillation, which terminate spontaneously and some of these are asymptomatic. According to your risk of stroke you may need lifelong anticoagulants even after your rhythm has been restored to normal.
Blood thinners (Anticoagulants)
Blood thinners are drugs that prolong the time of blood coagulation, preventing formation of thrombi (clots). Blood thinners could be vitamin K antagonists or non-vitamin K antagonist oral anticoagulant medications, also named new/novel oral anticoagulant (NOAC), or direct oral anticoagulant (DOAC).

Vitamin K antagonists
(warfarin, acenocoumarol, phenprocoumon)
Vitamin K antagonists are the oldest anticoagulants. They reduce the ability of the blood to form clots. If your doctor prescribes you one of these medications, you should carefully follow your doctor’s instructions.
You’ll need to have regular blood tests to monitor blood-thinning effects of the drug. This is measured by the “INR” or international normalized ratio. Normally in those not taking anticoagulants, blood clots with an INR of around 1. To reduce the risk of stroke in patients with atrial fibrillation the INR should be between 2 and 3. Depending on this measurement, the dosage of the drugs will be adapted on an individual basis. It is of utmost importance to perform this blood test regularly to make sure that the dosage you are using is correct and you are not at risk. The dosage used can differ from person to person and over time.
It is also important to know that foods containing high amount of vitamin K can counteract vitamin K antagonists. If your diet is high in vitamin K you will probably need to take more of the blood-thinning drug.
NOAC
These medications include dabigatran, rivaroxaban, apixaban and edoxaban. They are shorter acting than vitamin K antagonists and usually don’t require regular blood tests or monitoring by your doctor.
If you are prescribed NOAC, your kidney function has to be monitored by your physician. If the kidney function deteriorates, the medication dose may need to be lowered.
These medications can be used without monitoring the INR and are not influenced by food, other drugs and alcohol. Dabigatran and apixaban are taken twice a day and rivaroxaban and edoxaban can be taken once daily. It is extremely important that a NOAC is taken every day as prescribed by your physician.
Side effects
Risk of bleeding (with anticoagulant)
The most common side effect that occurs with all blood thinning medications is bleeding. In most cases bleeding is not serious, such as bruising or a minor nosebleed. About 1-2% of people on blood thinners will develop more serious bleeding which may require a blood transfusion and interruption of the blood thinning treatment. The most serious bleeding side effect from blood thinning medication is a bleed into the brain, known as an “intracranial hemorrhage”. If you are concerned about the risk of bleeding associated with your blood-thinning medication, please discuss this with your doctor. Your doctor will assess your individual risk of stroke and weigh up your risk of bleeding with a blood-thinning medicine.
Your doctor can calculate your risk of bleeding before you are offered one of the blood-thinning medicines using a risk score. One example of a commonly used bleeding risk score is the HAS-BLED score.
Assessing your risk of bleeding, if you are taking blood-thinning medications – online calculator
LAA occluders
Your doctor may also suggest a procedure to occlude the left atrial appendage (a pouch on the left upper chamber of the heart) where clots are often formed.
The procedure itself is conducted percutaneously, with local anesthesia. A catheter is inserted through a vein in the groin and placed in the upper left chamber (left atrium). A plug like device (left atrial appendage occluder) is delivered in collapsed form into the appendage and expanded to completely occlude the cavity of the left atrial appendage. The main purpose of closing the left atrial appendage is to prevent thrombi moving from the left atrial appendage to the left atrium and ventricle. This procedure is mainly recommended to patients who have increased risk of blood clots and a contraindication for anticoagulants because of very high bleeding risk (often because of previous life-threatening bleeding events).

 Français
Français Deutsch
Deutsch Español
Español Italiano
Italiano Nederlands
Nederlands Polski
Polski Русский
Русский Svenska
Svenska Português
Português Hrvatski
Hrvatski Ελληνικα
Ελληνικα 简体中文
简体中文 العربية
العربية